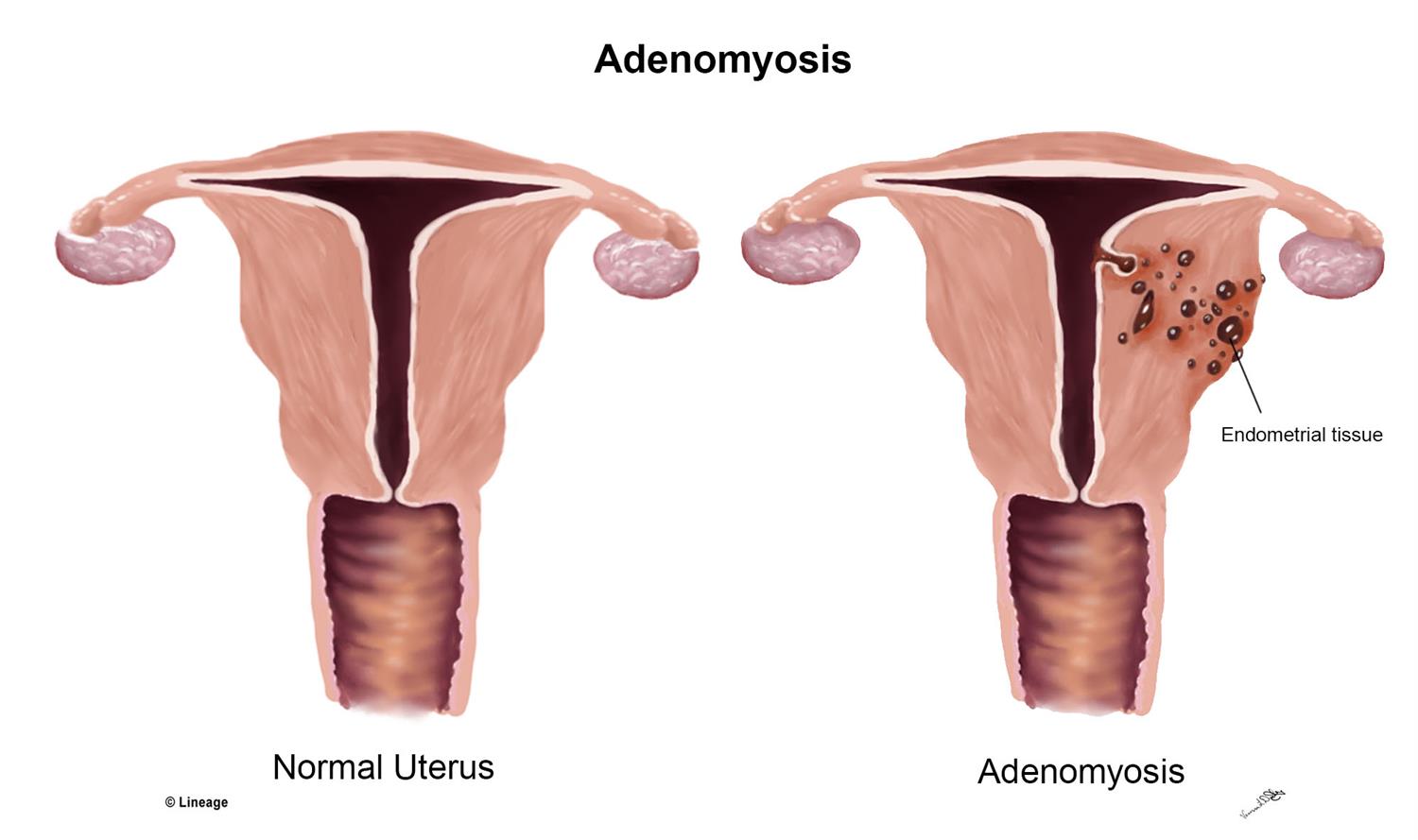
Adenomyosis is an enlarged uterus caused by growth of endometrial tissue into the uterine tissue. This means that the lining of the uterus grows into the wall and muscle (also called the myometrium) of the uterus. The tissue keeps working just like the uterine lining — it gets thicker and then breaks down every month during your period (1).

Is it dangerous to have an enlarged uterus?
In general, adenomyosis is not dangerous. In women with severe symptoms, however, heavy menstrual bleeding can lead to anemia, which causes fatigue. The excessive bleeding and pain can also lead women to avoid activities and socializing, which can strain relationships and lead to depression, anxiety and other emotional distress.
Can adenomyosis cause infertility?
In severe cases, adenomyosis that causes adenomyomas can lead to infertility in young women. (2) It is possible that adenomyosis itself can also cause infertility or trouble conceiving, but more research is needed. (3)
Possible problems conceiving may be due to the changes the disease can cause in the lining of the uterus or because it commonly co-occurs with endometriosis. (4) Adenomyosis and pregnancy are not necessarily incompatible, however. Many women with adenomyosis can conceive either naturally or with artificial assistance. (5) Normally, however, adenomyosis is diagnosed in women late in their childbearing years or after women have had children.
Is adenomyosis a cancer?
No, adenomyosis is not a type of cancer. However, adenomysois can result in a mass or lump of tissue called an adenomyoma. (6) These are basically benign (non-cancerous) tumors. They may look like uterine fibroids. Some people worry that adenomyosis and cancer of the endometrium or uterus may go hand in hand, but there doesn’t appear to be an increased risk of cancer among women with adenomyosis. (7, 8) Of course, some people with the condition will also have cancer, but it’s not believed that adenomyosis increases the risk. (9)
Can adenomyosis cause infertility?
In severe cases, adenomyosis that causes adenomyomas can lead to infertility in young women. (10) It is possible that adenomyosis itself can also cause infertility or trouble conceiving, but more research is needed. (11)
Possible problems conceiving may be due to the changes the disease can cause in the lining of the uterus or because it commonly co-occurs with endometriosis. (12) Adenomyosis and pregnancy are not necessarily incompatible, however. Many women with adenomyosis can conceive either naturally or with artificial assistance. (13) Normally, however, adenomyosis is diagnosed in women late in their childbearing years or after women have had children.
- Alter your diet
There is little specific research on diet and adenomyosis. However, many studies have investigated the relationship between diet and menstrual pain.
- Include omega-3 fatty acids: Endometriosis is more common in women with a lot of trans-fatty acids in their diet, and it is less likely in women who eat a lot of long-chain omega-3 fatty acids. (14) Since fish oil has also been found to reduce menstrual pain, it may make sense to eat a diet rich in omega-3 fatty acids and low in trans fats. (15, 16) Healthy sources of omega-3 fatty acids include fish such as mackerel and salmon, walnuts, chia seeds, flaxseeds, hemp seeds and egg yolks.
- Eat low-fat dairy: Abdominal bloating and pain during your period may be less likely if you eat three or four servings of dairy per day. (17)
- Consider a low-fat vegetarian diet: In a review of dietary and other treatments for painful and heavy periods, a low-fat vegetarian diet was identified as a possibly helpful way to reduce symptoms. (18)
- Eat lots of fiber: Women who ate a diet high in fiber had significantly less menstrual pain than women who didn’t in a Japanese study looking at multiple diets. (19)
According to the University of Maryland Medical Center, other dietary changes you can make to reduce period-related pain include: (54)
- Eat foods rich in calcium and antioxidants.
- Avoid processed or refined foods, such as white bread.
- Get your protein from lean meat, tofu or beans.
- Avoid caffeine and alcohol.
- Don’t smoke.
- Stay hydrated, drinking about six to eight glasses of water every day.
Conventional Treatment
Most women with adenomyosis do not require treatment. The condition is hard to diagnose and many times can only be confirmed after a hysterectomy. For women who are close to menopause, treatment may be less aggressive than for younger women unless symptoms are severe. This is because adenomyosis usually disappears after menopause, when estrogen levels drop. (23)
For women with adenomyosis symptoms, conventional treatment may include:
- Over-the-counter (OTC) anti-inflammatory drugs such as ibuprofen.
- Hormonal birth control. Pills that have a combination of estrogen and progestin or patches or rings that have this combination are sometimes prescribed to relieve pain and bleeding. Progestin-only pills or intrauterine devices can also cause periods to stop, which also stops period-related symptoms.
- Tissue destruction. Procedures such as endometrial ablation and MRI-guided focused ultrasound surgery try to destroy the endometrial tissue that is causing adenomyosis. These procedures may not work for everyone and more research is needed.
- Hysterectomy. This is surgical removal of the uterus. It permanently cures adenomyosis but is a major surgery. Adenomyosis hysterectomy is only done for women who have severe symptoms and who do not wish to have any more children.
Adenomyosis: 6 Natural Tips to Manage Symptoms
Natural treatments for adenomyosis generally involve managing the menstrual pain and bleeding caused by the condition.
- Try herbs and supplements
A wide variety of herbal remedies have been used throughout history and around the world for painful, long or heavy periods. Some options with research supporting their usefulness for pain relief, mood improvement, or bleeding reduction include:
- Valerian: A high-quality study found that valerian was effective at reducing pain during a period when given in 255 milligram doses three times per day for three days at the start of a period, for two periods in a row. The researchers believe the herb worked because of its antispasmodic effects.
- Rosa damascena (Damask rose): A study compared the use of a painkiller to Rosa damascena extract on painful periods. The two worked equally well and were effective in reducing pain intensity.
- Chinese herbal medicine: Some research suggests that combinations of Chinese herbs may help with painful periods. The most popular (based on prescriptions in Taiwan) are Corydalis yanhusuo, Cyperus rotundus, and Dang-Gui-Shao-Yao-San, or combinations containing these herbs.
- Rhubarb (Rheum emodi): Women taking capsules of rhubarb powder twice a day for two days before their period started and throughout the first three days of their period had a significant decrease in pain and its duration. In this study, other symptoms and quality of life were also better after taking the capsules to treat their period-related pain.
- Vitamin B1 and vitamin E: In a review of human studies, vitamin B1 at 100 milligrams per day was identified as an effective pain relief option for painful periods. A review of trials using herbal and dietary supplements to treat period-related symptoms found positive effects for women who had painful periods taking vitamin B1 and vitamin E. Please make sure to have an organic source of vitamin B’s. Beef liver capsules work well if you are unable to eat beef liver or chicken liver.
- Frankincense and myrrh: In a study in mice with painful periods (measured by signs of pain such as writhing), myrrh water extract, frankincense extract and a combination of the two were effective at reducing inflammation and pain. Although the doses in the study are not scaled for humans, the anti-inflammatory and pain-relief abilities of these herbs may also help women with painful periods.
- Magnesium: In a review of studies of natural pain relief for painful periods, magnesiumwas effective at reducing pain. However, the studies used different doses so there is no clear dose that is known to be the best option.
- Omega-3 fatty acids: In a small trial comparing fish oil to placebo pills, fish oil was more effective at relieving menstrual pain.
- Chamomile: In a large review of natural therapies for menstrual pain, one study was identified that found chamomile to be more effective than OTC non-steroidal anti-inflammatory drugs.
Other possible herbs and supplements with some support in terms of formal research include fenugreek, fennel, ginger, chasteberry, cumin, a combination of fish oil and vitamin B1, peppermint, “true” cinnamon or Cinnamomum zeylanicum, thiamine, pyridoxine, zataria, and zinc sulphate.
In general, however, there is virtually no data on safety. If you choose to use herbal remedies or supplements for menstrual pain or heavy bleeding, do so with caution. Consult a health care professional before you start any new herbs or supplements, since they can interact with other medications.
- Alter your diet
There is little specific research on diet and adenomyosis. However, many studies have investigated the relationship between diet and menstrual pain.
- Include omega-3 fatty acids: Endometriosis is more common in women with a lot of trans-fatty acids in their diet, and it is less likely in women who eat a lot of long-chain omega-3 fatty acids. Since fish oil has also been found to reduce menstrual pain, it may make sense to eat a diet rich in omega-3 fatty acids and low in trans fats. Healthy sources of omega-3 fatty acids include fish such as mackerel and salmon, hemp seeds ( in moderation) and egg yolks. Be sure to choose a high quality supplement of fermented cod liver oil for best absorption.
- Eat low-fat dairy: Abdominal bloating and pain during your period may be less likely if you eat three or four servings of dairy per day. (51)
- Consider a low-fat vegetarian diet: In a review of dietary and other treatments for painful and heavy periods, a low-fat vegetarian diet was identified as a possibly helpful way to reduce symptoms. (52)